by Issa Al Shamsi, SCHS Occupational Therapy
INTRODUCTION
Hirayama is a rare disease also known as benign juvenile brachial spinal muscular atrophy, juvenile asymmetric segmental spinal muscular atrophy (Lay, Gudlavalleti, & Sharma, 2023), cervical flexion myelopathy (Yen-Lin Huang, 2011) Commonly affects young men from Asia between the ages of 15-25 years old (Sharma, 2024).It’s a rare disease of nervous system, characterized by unilateral or bilateral atrophy and weakness of the distal upper extremity or the forearm and hands without sensory impairments of the affected area (Lay, Gudlavalleti, & Sharma, 2023). The disease causes difficulty for a patient to participate in activities of daily living due to weakness and joint stiffness.
EPIDEMIOLOGY
The disease was initially recognized by Keizo Hirayama in Japan in 1959 and commonly affects adolescence in Asian countries like Japan and India, (S. Anuradha, Case Reports In Neurologic Medicine, 2016) although there are some reported cases from Europe and North America (Lay, Gudlavalleti, & Sharma, 2023). The disease mainly affects young adults between the ages of 15-25 years of age (Al-Hashel, Abdelnabi, & Ismail, 2021), it predominantly affects males with a 20:1 male to female ratio (M. Agundeza, 2015).
ETIOLOGY
Although the cause of the disease remains unclear, forward displacement of the posterior cervical dural sac during neck flexion causes compression of the cervical cord and causes atrophic and ischemic changes in the anterior horn (Yen-Lin Huang, 2011). There are various pathophysiologic causes of Hirayama disease, such as (Saranya B Gomathy, 2022):
- Dysplasia of dural sac – irregularity in the growth of the spinal cord and spinal canal, which adds to the dura’s tightness, resulting in the spinal cord impinging on the vertebral column
- Nerve root dysplasia – The affected side’s posterior roots become tight. During neck flexion, the lower cervical cord on the affected side moves anteriorly and laterally as a result of the posterior roots’ inability to extend
- Spinal Ligament abnormalities – due to loss of elasticity of the fibers of the spinal ligament, epidural ligament causes tightness to the posterior dura
- Engorge posterior epidural venous plexus – When the neck is bent forward, a forward dural shift produces a negative pressure in the posterior epidural area, which impairs the return of blood, which results in ischemia in the cervical cord’s ventral nerve roots and anterior horn cells
CLINICAL FEATURES
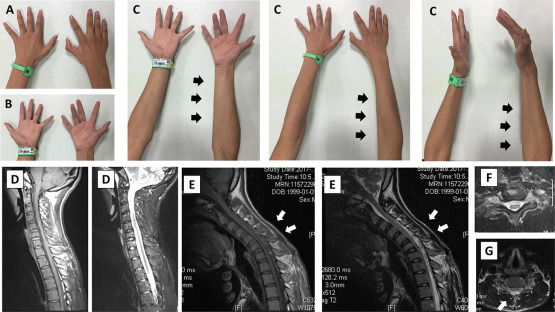
Hirayama disease often presents unilateral upper extremity weakness, atrophy, and cold paresis without sensory or pyramidal tract involvement (Sharma, 2024). Initially, a person with Hirayama disease notices difficulty performing daily activities such buttoning the shirt, holding or writing with a pen, mixing food and other activities of daily living that requires using of hand or upper extremity. (Bhat, 2020). According to Tashiro, there are five salient features of Hirayama disease (Saranya B Gomathy, 2022).
- Distal upper extremity weakness and atrophy predominantly on the ulnar side, unilaterally or bilaterally
- Tremors with polyminimyoclonus that are stiff and irregular in the afflicted fingers
- Acute symptoms worsen during cold weather or temperatures
- Often begins between the ages of 10 and 20 years old, progressing gradually over the course of 3 to 5 years before ceasing of symptoms
There are no signs of sensory loss or electromyographic (EMG) alterations on the affected extremity that indicate chronic denervation

Photo source: https://www.modernghana.com/lifestyle/14499/all-you-need-to-know-about-hirayama-disease.html. By Dr. Dhananjaya I Bhat, Senior Consultant, Neurosurgery, Aster RV Hospital
It is observed in this photo that the right hand has muscle atrophy with noticeable clawing, due to joint stiffness and weakness of the hand muscles.
EVALUATION AND EXAMINATION
The most important diagnostic instrument in assessing a patient who may have Hirayama disease is an MRI of the cervical spine region in neutral and flex positions (Saranya B Gomathy, 2022). In a neutral position, the cervical spine may appear normal. However, during the flex position, anterior displacement of the posterior dura mater is evident, which is essential for properly determining the diagnosis (Julian Llano, 2020). Hirayama disease is diagnosed based on clinical signs of MRI/Flexion MR characteristics, which include segmental spinal cord atrophy, widening of the posterior epidural space, and elevated T2-weighted intramedullary cord signal (Karol Galletta, 2020). During the nerve conduction test, the mean ulnar/median CMAP amplitude is significantly less in Hirayama disease, differentiating it from ALS, which is abnormally high when compared to normal subjects (Al-Hashel, Abdelnabi, & Ismail, 2021).
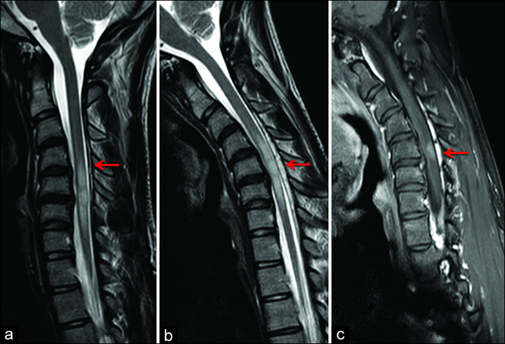
Photo source: Surgical Neurology International (Karol Galletta, 2020)
(a) Sagittal T2-weighted FSE image in neutral position with evidence of posterior detachment of dural sac (arrow). (b) Flexion sagittal T2-weighted FSE images confirming anterior displacement of the posterior dura from C4 to C7 levels with spinal cord flattening and prominence of the posterior epidural space (arrow). (c) Sagittal contrast-enhanced T1-weighted FSE in flexion position with evidence of enhancement of the enlarged posterior epidural space (arrow).
PROGNOSIS
Despite the fact that Hirayama disease is a self-limiting condition, early detection is essential (Atul T Tayade, 2010). Hirayama disease usually stops progressing after 1–5 years from the onset of the disease (Al-Hashel, Abdelnabi, & Ismail, 2021). The patient usually received conservative treatments, which included a cervical collar to be worn constantly and regularly (Julian Llano, 2020).
TREATMENT
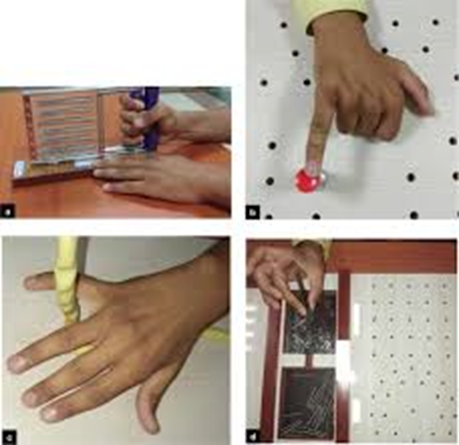
Rehabilitation treatment is an advantage; it helps prevent complications from prolonged immobility such as muscle wasting and joint stiffness (S. Anuradha, Case Reports in Neurological Medicine, 2016). Another goal for rehabilitation is to improve the strength of the posterior cervical extensors, resulting in an improvement in cervical sagittal alignment (Lay, Gudlavalleti, & Sharma, 2023) which would decrease the pressure on the affected vertebral root. Strengthening exercises are one of the most important treatment for this disease to improve hand grip and enhance activities of daily living participation. (Mishra, n.d.).
According to a case study that focused on the effect of strengthening exercises with Hirayama disease (Tinu Sethi, 2020). An 18 year-old male received hand strengthening exercises for 40 minutes, 5 days a week for a period of 8 week. During the exercise, the patient used tools such as Thera putty, gel ball, finger dexterity board and hand grip exerciser. After the program, the patient was assessed using manual muscle testing, hand-held dynamometer, pinchometer and the Minnesota Manual Dexterity Test. The results showed significant increase in strength and hand functions.
A surgical procedure is indicated when there is a rapid progression of severe illness, positive pyramidal symptoms, poor neck collar compliance, and failure of conservative treatment (Saranya B Gomathy, 2022). However, supporting surgical treatment is extremely challenging because of the rarity of Hirayama disease (M. Agundeza, 2015).
References
Al-Hashel, J. Y., Abdelnabi, E. A., & Ismail, I. I. (2021, December). Case Reports in Neurology. Retrieved from Karger: https://karger.com/crn/article/12/3/291/97526/Monomelic-Amyotrophy-Hirayama-Disease-A-Rare-Case
Atul T Tayade, S. K. (2010). PubMed Central. Retrieved from National Library for Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3137836/#:~:text=This%20disease%20was%20described%20first,and%20is%20often%20self%2Dlimited.
Bhat, D. D. (2020). All You Need To Know About Hirayama Disease. All You Need To Know About Hirayama Disease.
Julian Llano, N. U. (2020, June). Ochsner Journal. Retrieved from Ochsner Journal: https://www.ochsnerjournal.org/content/20/2/117
Karol Galletta, M. G. (2020). Hirayama disease . Early MRI diagnosis of subacute medullary ischemia: A case report. .
Lay, S., Gudlavalleti, A., & Sharma, S. (2023). StatPearls. Retrieved from National Library of Medicine: https://www.ncbi.nlm.nih.gov/books/NBK499913/
M. Agundeza, I. R. (2015). Neurolgia. Retrieved from Elsevier: https://www.elsevier.es/en-revista-neurologia-english-edition–495-articulo-hirayama-disease-is-surgery-an-S2173580815001145
Mishra, R. (n.d.). https://www.physio-pedia.com/Hirayama_Disease. Retrieved from https://www.physio-pedia.com/: https://www.physio-pedia.com/Hirayama_Disease
S. Anuradha, V. F. (2016). Case Reports In Neurologic Medicine. Retrieved from Hindawi: https://www.hindawi.com/journals/crinm/2016/5839761/
S. Anuradha, V. F. (2016). Case Reports in Neurological Medicine. Retrieved from Hindawi: https://www.hindawi.com/journals/crinm/2016/5839761/
Saranya B Gomathy, A. A. (2022, November). Neuromuscular Diseasea. Retrieved from Touch Neurology: https://touchneurology.com/neuromuscular-diseases/journal-articles/hirayama-disease-review-on-pathophysiology-clinical-features-diagnosis-and-treatment/
Sharma, R. (2024, January 13). Radiopedia.org. Retrieved from Radiopedia.org: https://radiopaedia.org/articles/hirayama-disease
Tinu Sethi, S. R. (2020). International Journal of Therapy and Rehabilitation. Effect of strengthening exercises in Hirayama disease: a case study.
Yen-Lin Huang, C.-J. C. (2011). Pub Med. Retrieved from National Library of Medicine: https://pubmed.ncbi.nlm.nih.gov/22032508/#:~:text=Hirayama%20disease%20(juvenile%20muscular%20atrophy,spontaneous%20arrest%20within%20several%20years.